The Ethical Frontier: Synthetic Human Embryos and the Controversial Potential for Extended Research
In an era of groundbreaking biomedical research, the creation of synthetic human embryos using stem cells, as revealed by developmental biologist Magdalena Żernicka-Goetz during the 2023 International Society for Stem Cell Research (ISSCR) annual meeting, is opening up new avenues for investigation. These synthetic embryos could revolutionize our understanding of
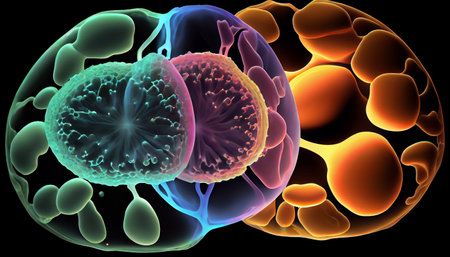
In an era of groundbreaking biomedical research, the creation of synthetic human embryos using stem cells, as revealed by developmental biologist Magdalena Żernicka-Goetz during the 2023 International Society for Stem Cell Research (ISSCR) annual meeting, is opening up new avenues for investigation. These synthetic embryos could revolutionize our understanding of human development, genetic disorders, fertility treatments, and even the potential for reproduction without conventional means. However, they also navigate uncharted ethical waters.
Synthetic human embryos, also known as embryoid bodies, embryonic models, or embryo-like structures, emulate the development of natural human embryos, i.e., those generated through fertilization. These synthetic versions include cells that usually form the embryo, placenta, yolk sac, and develop precursors of germ cells (future sperm and eggs).
Research involving these synthetic entities is less controversial for some, primarily because they cannot develop into postnatal stage humans - they are non-viable and do not result in live births. This nature of synthetic embryos could theoretically allow research to extend beyond the internationally recognized 14-day limit applied to natural human embryos. However, the practicality and ethical permissibility of this extended research is a topic of intense debate.
The research conducted by Żernicka-Goetz adhered to the Human Fertilisation and Embryology Act of 1990 in the United Kingdom (UK), which imposes a 14-day limit on human embryo research. As synthetic embryos are not created by fertilization, the Act does not apply to them, allowing research beyond the 14-day limit.
The situation is different in Canada, where the Assisted Human Reproduction Act (AHR Act) encompasses both natural and synthetic human embryos in its definition, without stipulating a specific method of creation. Therefore, the Act applies to synthetic human embryos as well, provided they qualify as human organisms. This definition leads to restrictions on the creation and use of synthetic human embryos in Canada, which are bound by the same 14-day rule as natural embryos.
Advocates of extended synthetic human embryo research could argue that the AHR Act's definition of "human embryos" does not encompass synthetic ones, or assert a significant moral distinction between natural and synthetic embryos due to the latter's non-viability. However, such arguments seem to have little ground, given the Act's current wording and political reluctance to alter it.
These complex ethical considerations demonstrate the challenges faced in the fast-evolving realm of stem cell research. The potential benefits of synthetic human embryo research are enormous, but ensuring this progress aligns with our moral and ethical boundaries remains paramount. While synthetic human embryos may be the new frontier in stem cell research, the future of this exploration will heavily rely on how we navigate these ethical dilemmas.